photo credit: Une tétine. / A pacifier. via photopin (license)
photo credit: Une tétine. / A pacifier. via photopin (license)
Have you ever heard the pitch from a sex education abstinence program? The leaders of this type of program encourage high school students to not become sexually active. “Just don’t do it -wait until you’re older/married” is the message that teens take in. And if you’re like me (the mom of a future high school student), this probably sounds like the best advice you’ve ever heard. The only problem is, this kind of teaching doesn’t work to stop kids from having sex. For many high school students, it’s just not realistic that they will choose to abstain altogether. After all, there is a monsoon of hormones swishing around, intense situations, and the urge to find some relief from pent up frustrations. Because of these factors, some teenagers will become sexually active, no matter how much we don’t want them to. And if they are having sex without being safe about it, some negative consequences might occur. In this case, we are mainly worried about pregnancy and STDs. So if we know this to be the reality, why not teach them how to lower their risks for problems if they choose to become sexually active? And in fact, this country is starting to move away from abstinence teaching and towards contraception teaching as the national standard. We hope to see the rate of unintended pregnancies and STDs drop as a result.
I find that pacifier teaching bears a strong resemblance to abstinence teaching. A similar message of “just don’t do it – wait until the baby is at least one month old” is preached to new moms. And just like with abstinence education, telling a mom to avoid the pacifier initially sounds like great advice. If we can get a baby to suck only at the breast, especially during the first few days/weeks of life, we can expect an adequate milk supply and healthy weight gain. So holding off on the binky for a few weeks is a worthy goal, with solid reasoning behind it. However, avoiding the pacifier altogether doesn’t always mesh well with the reality of living with a newborn. And just like the teens who thought they might be able to abstain from sexual activity but got involved anyhow, many moms end up using a pacifier even if it wasn’t their original intention. (After all, there is a monsoon of hormones swishing around, intense situations, and the urge to find some relief from the pent up frustrations.) I’ve had many moms say something to the effect of, “I know it’s bad to use the binky, but it’s been helping us all to cope!” And so these moms give their babies pacifiers without any knowledge of “safe pacifier use”…. and some negative consequences might occur. In this case, the main concern is how pacifier use might interfere with establishing a milk supply.
Considering what’s at stake (a happy and healthy breastfeeding relationship) and the reality of the situation (many moms choosing to use a pacifier) I want to pose the question – is it possible to use a pacifier in the early days and limit or avoid negative outcomes?
What would happen if, like with sex ed, we shifted from a “just don’t do it” message to more of a “if you decide to use a pacifier, here is how you can help to protect breastfeeding” message? I would hope to see fewer negative consequences resulting from pacifier use. I don’t see the down side of a more forthcoming manner of teaching, as we know that many moms are using the pacifier despite the prevalent “just don’t do it” message.
 photo credit: Sagan – Binky Obsession via photopin (license)
photo credit: Sagan – Binky Obsession via photopin (license)
The American Academy of Pediatrics says:
“For breastfed infants, delay pacifier introduction until 1 month of age to ensure that breastfeeding is firmly established.”
And I would like to add that if you decide to use one anyway, please keep in mind:
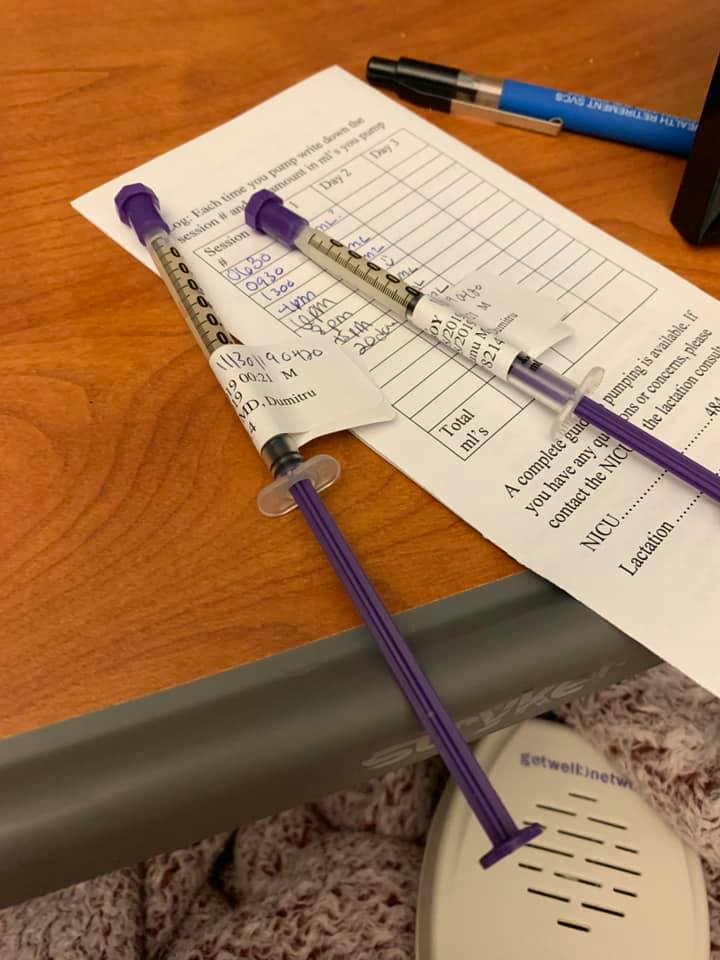
Rule #1. Limit the pacifier during the first few days of life. Making milk is a simple case of supply and demand, and it is your baby’s job to tell your body to make milk. Your body is in an especially sensitive period in the hours and days after you deliver. The more you allow your baby to suck on the breast, the greater a supply of milk you will make. The less that your baby is sucking on the breast, the less milk you will make. Some babies take their job very seriously, and want to be on the boob for what feels to mom like a 24/7 shift. Moms with a baby like this may feel overwhelmed and tired of having their baby not be content unless he has a boob in his mouth. They want a break, they need a shower, they need two hands to eat their cheeseburger, and they need to put the baby down to sleep so that everyone can sleep safely. And after using the pacifier to get a little breathing room and perhaps take a nap, I would hope that a mom like this feels refreshed enough to give her baby his boob back.
So as long as your baby is feeding well 8-12 times in a day and putting out the correct amount of diapers, limited pacifier use shouldn’t be a milk-making deal breaker. You can always choose to hand express/pump a little, too, if you feel as though your body has been missing out on “make milk” signals.
Once your milk increases in volume (usually around day 3), continue to ensure 8-12 good feedings at the breast, watch for signs that baby is getting enough, and use the pacifier as desired when you really need a break but baby wants to suck. Another good time to consider the pacifier is when you know baby wants to eat but he will have to wait a few minutes and you want to keep him calm in the meantime. For example, you’re in the shower and the baby is trying to latch on to dad, or, the baby is screaming in the carseat and your boobs just aren’t that flexible.
Rule #2. Get help if you are using a pacifier due to very sore nipples. Some moms start using the pacifier because their toes curl in pain at the mere thought of breastfeeding. A mom like this puts her baby on the breast for only as long as she can stand it and then he gets cut off. But he immediately starts crying and tries to go back on. Instead of her own nipple, the mom gives her baby his binky, which settles him and he falls asleep. Mom breathes a deep sigh of relief, but she has actually just made things worse for herself in the long run. Because the baby is sucking on the pacifier instead of her breast, her body decides to downgrade the milk supply. With less milk available, the baby will be hungry more often and will want to spend more time nursing, which is a terrible fate for a mom with sore nips.
If you are having intense nipple pain, there is something going on with the latch, baby’s suck, or both. And an IBCLC is probably the best person to help you. So, if you are using the pacifier to give your nipples a vacation, continue to use the pacifier, but definitely start pumping (and bottle feeding) to replace your baby’s demand, and get some help!
Rule #3. Don’t use the pacifier because you think your baby is eating too often. Moms in this camp look at their baby giving clear hunger cues and say “You just ate an hour ago so you’re not due to eat for at least another hour.” In goes the binky, and then maybe mom latches the baby in an hour or two. Or maybe the baby falls asleep and sleeps for 2-3 hours. Either way, this mom’s body just received a very clear signal to “make a little less” when baby would have been happy to spread the “make a little more” message. It is not possible to overfeed your baby in the first few days. Your baby has a tiny tummy and you are making small amounts of colostrum (newborn milk) which baby has to work very hard to extract. If your baby is giving clear hunger cues, put him back onto the breast, irregardless of when you fed him last. Watch your baby and not the clock. If this starts to get overwhelming, refer back to Rule#1 for some guidance and seek help from an IBCLC.
 photo credit: Baby Ben with Uncle Ben via photopin (license)
photo credit: Baby Ben with Uncle Ben via photopin (license)
I hope that you now have a better understanding of why the “just don’t do it” message exists, and how holding off on the pacifier for a few days is typically a good move if you want to meet your breastfeeding goals. But if you must, please practice “safe pacifier use”….and spread the word!